Parotitis PATHOGENESIS, MICROBIOLOGY, DIAGNOSIS

Parotitis is inflammation of the parotid salivary gland: it can be acute, chronic, or chronic with acute exacerbations. Acute suppurative parotitis was a well recognized complication of abdominal surgeries prior to routine administration of perioperative antibiotics. The incidence of parotitis has been reported to be 0.01%-0.02 % of all hospital admissions and 0.002%-0.04% of post operative patients. The etiology of parotitis is assumed to be ascending infection from the oral cavity. Many risk factors are associated with acute parotitis based on patient population with dehydration being the most significant. Staphylococcus aureus is the most common bacterial pathogen; however anaerobes and mixed infections are increasingly being identified. Treatment includes antimicrobials, hydration, and excluding an obstructive process within Stensen’s duct that would warrant intervention.
PATHOGENESIS
Acute bacterial parotitis occurs mostly in neonates and in elderly or debilitated persons with systemic illness or after surgery. Predisposing conditions include: dehydration, malnutrition, immunosuppression, dental infections, tracheostomy, and medications that suppress salivary flow (antihistamines, diuretics, anticholinergic medications). Bacteria spread from the oral cavity to the parotid gland via Stensen’s duct. Another potential mechanism, especially in newborns, is hematologic spread from transient bacteremia.
Chronic bacterial parotitis may exist in the presence of calculi or stenosis of the ducts secondary to injury, and less likely as a sequela of acute bacterial infection. In most instances, the chronic disease is autoimmune with superimposed bacterial infections.
Viral parotitis is more common worldwide than bacterial parotitis with mumps being the most common viral cause of parotitis in children. Other viruses are provided in Table.
MICROBIOLOGY
Historically, Staphylococcus aureus has been the most common pathogen associated with bacterial parotitis, accounting for 80% of cases. Recent studies have suggested mixed infections including streptococci, anaerobes, and gram-negative bacilli. Other bacterial causes are provided in Table 1. There is no correlation between predisposing conditions and the inciting pathogen, except the association of anaerobic with dental infections.
Candida associated parotitis has been observed in hospitalized or institutionalized patients with poor mouth care, but is uncommon. In chronic parotitis, infection with Staphylococcus spp. or mixed infection with oral aerobes and anaerobes is common.
DIAGNOSIS
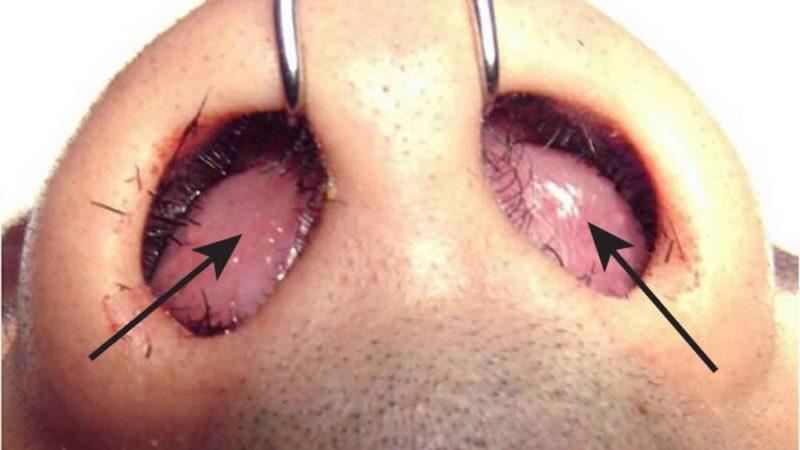
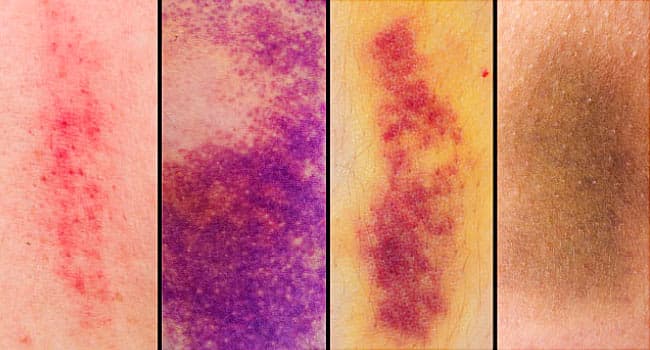
The diagnosis is clinical. Acute parotitis presents with sudden onset of indurated, warm, erythematous swelling see photos of the pre- and post-auricular areas, with intense local pain and tenderness. Symptoms are often associated with high fevers, chills, and marked systemic toxicity. The infection is usually unilateral; bilateral infections are more associated with neonatal cases. Purulence from the gland see photos and Gram stain may support the diagnosis of acute suppurative parotitis. Cultures may be obtained from parotid needle aspiration.
Late in the course of the infection, massive swelling of the neck and respiratory obstruction may occur. Other late manifestations include septicaemia, osteomyelitis of adjacent bones, and organ failure.
Sialography in contraindicated in the acute stage of infection due to the risk of rupture of an ectatic duct from the pressure of injected dye and usually incites intense pain. Ultrasound is replacing sialography in the evaluation as it is easier to perform, demonstrates solid masses or fluid collections within the gland, and detects hypoechoic areas that correspond to punctate sialectasis by sialography. CT scanning and MRI with gadolinium enhancement may be used to determine the size, shape, and presence of a neoplasm or abscess within the gland.
DIFFERENTIAL DIAGNOSIS
Bacterial parotitis must be differentiated from viral parotitis which is most commonly caused by mumps; other viral pathogens include HIV, enteroviruses, EBV, influenza, parainfluenza, CMV, and lymphocytic choriomeningitis. Non-infectious disorders associated with parotid swelling include collagen vascular disease, cystic fibrosis, sialolithiasis, diabetes, uremia, sarcoidosis, and tumors. Chronic may be confused with Sjögren syndrome, a non-infectious condition characterized by the triad of xerostomia, keratoconjunctivitis, and systemic autoimmune disease.
Bacterial parotitis must be differentiated from chronic recurrent parotitis, a condition more common in children but could persist into later life. The key to successful treatment for this condition is rapid and complete removal of the inspissated proteins particles in the duct, as well as steroids to suppress the inflammatory response (1).
MANAGEMENT OF PAROTITIS
Adequate hydration and antimicrobial therapy are the main stay of treatment. Antibiotics should be administered intravenously in acute bacterial parotitis after obtaining blood cultures. Staphylococcus aureus is the most common organism in community-acquired parotitis and first-line antibiotic therapy should include antistaphylococcal antibiotic (nafcillin, oxacillin, cefazolin). MRSA coverage should be considered if the patient has a history of recurrent cutaneous MRSA abscesses, residence in a nursing home with endemic MRSA, or other predisposing condition. For health care associated parotitis, broad spectrum antibiotics are recommended as mentioned in Table. Cefoxitin, imipenem, ertapenem, the combination of a penicillin plus beta-lactamase (amoxicillin/clavulanate, ampicillin/sulbactam) will provide adequate coverage. However, the presence of MRSA may mandate the use of vancomycin, linezolid, or daptomycin. The presence of associated dental infection warrants anaerobic coverage. In penicillin allergic patients, clindamycin is an alternative option.
Treatment should be adjusted based on culture results and presence or absence of bacteremia. Standard therapy is 10 to 14 days, likely longer in the presence of bacteremia. Surgical drainage and decompression of the gland are occasionally required if spontaneous drainage does not occur. Therapy for chronic parotitis should initially be conservative. Parotidectomy may eventually be required for people with long-standing infection. Good oral hygiene, adequate hydration, and early therapy for bacterial infections of the oropharynx are helpful measures for preventing acute bacterial parotitis.