Left Acute Viral Parotitis

A 10-year-old kid introduced parotitis to the crisis office (ED) with 2 days of left-sided face and neck torment, enlarging, and second rate fever. He had been seen the day preceding at an otolaryngology center for the indications and had been set on cephalexin, sialagogues, and back rub of the left parotid region. Regardless of treatment, his manifestations kept on declining, with expanded torment and enlarging, and he was alluded to the ED for worries of parotitis.
His previous history was critical for careful fix of congenital fissure and sense of taste, ear medical procedures with tympanostomy tube positions, left mastoidectomy, and constant ear seepage.
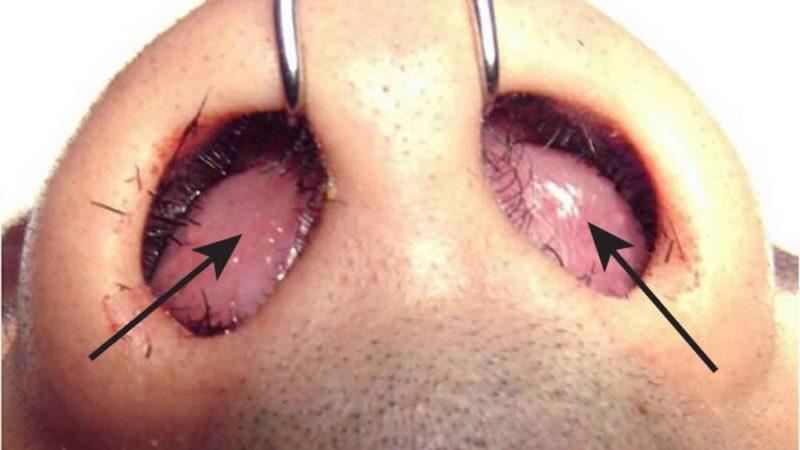
Upon assessment in the ED, the kid had a temperature of 36.7°C, a beat of 112 beats/min, and a respiratory pace of 28 breaths/min. Relevant clinical discoveries incorporated a 6 × 5-cm space of diffuse, nonerythematous, delicate, delicate, nonfluctuant, edematous, enlarging of the left half of the face, reaching out from the point of mouth to the preauricular region, and from the point of the left jaw down to the upper piece of neck, with delicacy over the back part of the expanding.
The left parotid conduit was marginally edematous, with no substantial mass or stone in the pipe, as indicated by the otolaryngologist’s report from the earlier day. Various little front cervical hubs were obvious, to a greater degree toward the left side than on the right. Scarred, thickened tympanic films were envisioned reciprocally. The remainder of the assessment discoveries were ordinary.
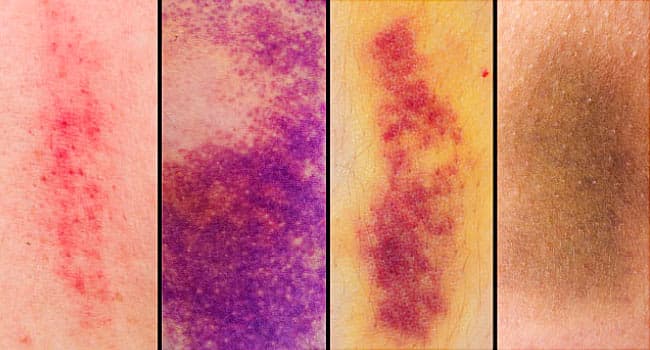
The absolute white platelet count was 16,000/µL with 76% neutrophil power, the C-receptive protein level was 1.75 mg/dL, and the amylase level was 590 U/L; blood was sent for bacterial culture. Ultrasonography assessment of the space showed an echogenic, lopsidedly augmented, edematous left parotid organ, with round hypoechoic foci inside, addressing intraparotid lymph hubs (B and C) and left cervical chain hubs, without proof of canker development.
In light of clinical discoveries, research facility reports, and ultrasonography reports, the patient got a conclusion of left intense parotitis. The patient was treated with intravenous clindamycin 300 mg and intravenous dexamethasone 8 mg and was conceded to the emergency clinic for perception. Bacterial culture was accounted for negative, and a last determination of viral parotitis was made. The kid was sent home with a 10-day routine of oral clindamycin.
Conversation
The etiology of parotid expanding can be irresistible or noninfectious. The unexpected beginning of an indurated, warm, erythematous enlarging of the cheek reaching out to point of jaw is normal for intense parotid contamination. Plague mumps brought about by paramyxovirus is the most widely recognized reason for viral parotitis among youngsters. Difficult parotitis happens in 60% to 75% of diseases and in 95% of patients with symptoms.1
Normally, parotid organ expanding begins with a short prodromal period of second rate fever, anorexia, discomfort, and cerebral pain; it then, at that point, advances more than 2 to 3 days and perseveres for about seven days. The level of agony and delicacy of the expanding is identified with the movement and goal of parotitis.
Beside paramyxovirus, other viral reasons for inconsistent enlarging incorporate coxsackievirus A, Epstein-Barr, flu A, and parainfluenza. The differential finding for parotid extension incorporates adolescent repetitive parotitis, cystic adenitis, dental boil, Ludwig angina, tainted growths, sialolithiasis, cystic fibrosis, sarcoidosis, collagen vascular problems, and lymphoma. Inclining factors remember a septic concentration for the oral pit, drying out, hunger, immunosuppression, and the utilization of antihistamines and diuretics.
The determination of parotitis is basically clinical. Sonography of the organ might assist with affirming the determination and preclude boil development. Heights of white blood count, erythrocyte sedimentation rate, C-responsive protein level and serum amylase level are seen in patients with suppurative parotitis. Serum amylase is raised in 90% of patients, separates parotitis from adenitis, and is definitely not a particular sign of viral parotitis.2 Raising serum immune response titers typically recognize viral causes once the intense scene dies down.
Support of good oral cleanliness and sufficient hydration and the organization of wide range parenteral anti-toxins to cover vigorous and anaerobic microbes might lessen the event of suppurative parotitis.