Acute Neonatal Suppurative Parotitisi: A Case Report
Neonatal suppurative parotitis (NSP) is an extremely uncommon sickness of the salivary organs, ordinarily including the parotids. It is generally because of Staphylococcus aureus bacterial disease among patients with inclining variables, and the board basically depends on hydration and intravenous anti-microbials with a great anticipation. Thus, we present an instance of a 11-day-old female child who gave left periauricular edema and delicacy related with fever that was subsequently analyzed as NSP because of both non-typable beta-hemolytic streptococci and Escherichia coli.
Anti-toxins treatment (vancomycin and gentamicin) was begun, and the patient recuperated totally following nine days. The CAse REport (CARE) rules were observed for announcing our case. Our case emphasizes the way that NSP ought to be in the differential conclusion of any child giving fever and parotid region enlarging. Brief analysis is fundamental for early administration with anti-infection agents and to keep away from confusions.
Presentation
Neonatal suppurative parotitis (NSP) is an uncommon illness of the salivary organs, generally including the parotids, with an expected commonness of 3.8 per 10,000 cases. In forty years, just 32 instances of NSP have been distinguished, as revealed in a concentrate by Spiegal et al. NSP is most ordinarily brought about by Staphylococcus aureus microscopic organisms yet may likewise be expected to other bacterial separates, for example, Escherichia coli, Pseudomonas aeruginosa, and bunch B streptococci.
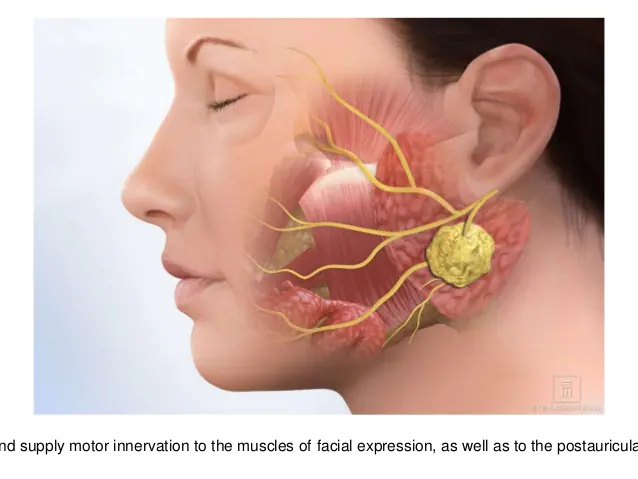
Obsessively, the advancement of NSP has been accepted to happen due to hematogenous cultivating of the organ or climbing disease from the oral depression through the Stensen’s conduit, which leaves the parotid organ before the pinna, and runs underneath the zygomatic curve over the masseteric muscle. A few factors that increment the danger of procuring the contamination incorporate injury to the oral hole, diminished insusceptibility or immunodeficiency, parchedness, hindrance of the Stensen’s channel, primary glandular irregularities, low birth weight, sepsis, nasogastric intubation, and hunger. The executives depends essentially on hydration and intravenous anti-microbials and infrequently needs careful mediation.
We report the instance of a 11-day-old Lebanese female child determined to have neonatal suppurative parotitis because of non-typable beta-hemolytic streptococcus bacterial disease and oversaw effectively with anti-toxins. Furthermore, we talk about the differential findings and helpful methodologies carried out in treating this case and comparable cases. This case report was led and announced as per the CAse REport (CARE) rules for revealing case reports.
Case Show
A 11-day-old full-term child young lady brought into the world at 40 weeks of growth by C-area and birth weight of 2780 g to a 33-year-old mother (G1P0A0; who guaranteed a smooth course of pregnancy (aside from tooth extraction because of dental boil seven days before conveyance treated with amoxicillin-clavulanic corrosive anti-microbial) with no perinatal and post pregnancy entanglements) was conceded to the crisis division because of one day of fever (twice coming to above 38°C as estimated by the mother at home), and enlarging in the left periauricular locale. Facial or head injury, maternal mastitis, or other maternal skin disease (as the patient was solely breastfed, and this may be a wellspring of contamination) were prohibited after the underlying appraisal. No perinatal inconveniences and no pertinent maternal or familial history had been accounted for.
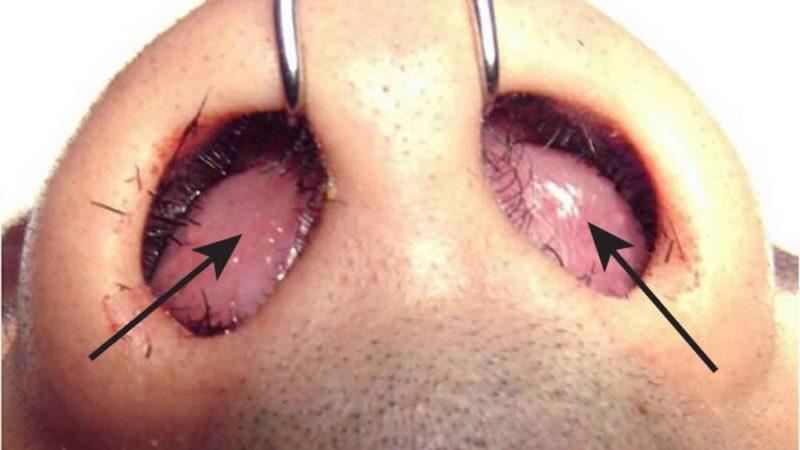
On actual assessment, the patient was dynamic. Neighborhood fiery signs at the left periauricular district were seen, including hotness, redness, and delicacy, with unbending nature covering a space of around 1 × 1 cm. Mouth and ear assessments showed purulent release at the Stensen’s conduit. Swab and blood societies were taken.
Lab tests showed a hemoglobin level of 14.3 g/dL (reference range: 12.5-21.0 g/dL), hematocrit level of 43.0% (reference range: 39.0% to 60.0%), white platelet count of 25.3 × 103/μL (reference range: 5.0 to 21.0 × 103/μL) with 63.0% neutrophils, 23.1% lymphocytes, 11.5% monocytes, 1% basophils, and 1.4% eosinophils, platelets count of 491 × 103/μL (reference range: 150 to 450 × 103/μL), and C-receptive protein level of 9 mg/L (reference range: 0 to 6 mg/L). Serum alpha-amylase fixation was 11 IU/L (reference range: 25 to 125 IU/L). Other research center tests, including electrolytes, urea, and creatinine, were not critical.
Ultrasound assessment of the left parotid and preauricular locale uncovered an amplified and edematous left parotid organ with expanded interior Doppler movement proposing left parotitis. The left parotid organ estimated 3.66 × 1.57 cm. Nearby subcutaneous edema was noted. The right parotid organ seemed typical in size and echotexture with ordinary Doppler action and no indications of fiery changes.
Thinking about the clinical show and ultrasound discoveries, the young lady was determined to have left intense suppurative parotitis. She was hospitalized, and an intravenous exact anti-microbial treatment with vancomycin (50 mg/kg/day) and gentamicin (7.5 mg/kg/day) was started. Additionally, absense of pain with paracetamol and intravenous liquid treatment was carried out. Following one day of parenteral treatment, her fever died down, and on the fourth day of treatment, the parotid expanding essentially lessened. Blood societies returned negative while the Stensen’s conduit exudate culture returned positive for non-typable beta-hemolytic streptococci and Escherichia coli touchy to the established anti-infection.
Conversation
Diseases of the salivary organ are not normal in children, but rather in the event that they happen, they include the parotid organ by and large. NSP is an uncommon illness that influences the parotids singularly (in 77% of cases) joined by expanding (77%) with or without redness and radiated discharge from the ipsilateral Stensen’s channel. The major causative specialist is Staphylococcus aureus (61%). Conclusion of NSP is principally clinical, despite the fact that ultrasound assessment of the parotid and preauricular area is normally performed to affirm the analysis and preclude boil development. Three demonstrative measures of suppurative parotitis were depicted in 1970 by David et al. that include:
(I) parotid expanding,
(ii) purulent exudation from the Stensen’s conduit,
(iii) development of pathogenic microorganisms in a culture of the discharge. In any case, in any presumed NSP, an overall sepsis workup should be done alongside ultrasound of the parotid organ and otolaryngology and irresistible illness interviews
In a concentrate by Ismail et al. distributed in 2013, including 44 announced instances of NSP somewhere in the range of 1970 and 2013, men established 77% of patients. Fever was just seen in 47% of cases, and rashness was available in 33% of the patients. In a similar report, it was shown that the backbone of parotitis treatment was a blend of hostile to staphylococcal anti-toxins with either an aminoglycoside or a third-age cephalosporin. Since clinical treatment delivers high achievement rates, there is no requirement for careful mediation as a rule.
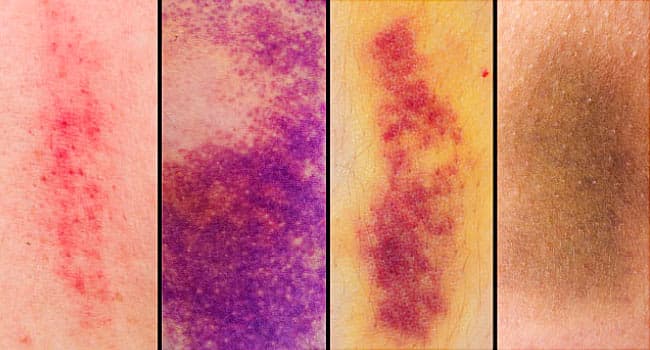
In contrast to most announced cases, our patient was a young lady. The patient was febrile on affirmation with expanding in the left parotid district. She had fringe leukocytosis with expanded neutrophil count reminiscent of an irresistible interaction because of a bacterial microbe. The differential determination included lymphadenitis, cellulitis, mumps parotitis, delicate tissue ulcer, mastoiditis, and non-irresistible etiologies like innate oddities (hemangioma or venolymphatic abnormality of the parotid organ).
In spite of the fact that Staphylococcus aureus is the most as often as possible segregated microorganism in societies, discharge societies for our situation were positive for both non-typable beta-hemolytic streptococci and Escherichia coli. Curiously, and dissimilar to most cases announced in world writing, discharge culture was positive in our patient to two microscopic organisms. She was breastfed, raising the worry that she may have gotten the contamination from her mom (through maternal mastitis or other maternal skin disease); in any case, the last option was rejected. To make and affirm the conclusion, ultrasound was performed to reject different elements that may have inclined the patient to foster NSP like Stenson’s channel anomaly, sialolith, and parotid organ neoplasm.
For our situation, vancomycin and gentamicin were allowed for nine days alongside forceful hydration, after which the patient was released home with complete recuperation following two months follow-up. In certain reports, possible complexities of NSP have been accounted for, like osteomyelitis of the mandible or temporomandibular joint, thrombophlebitis of the jugular vein, respiratory check, and sepsis.
Ends
NSP is extremely uncommon in youngsters. Our case emphasizes the way that NSP ought to be in the differential determination of any youngster giving fever and parotid region expanding. Brief finding is vital for early administration with anti-infection agents and to stay away from intricacies.